Central Sleep Apnea Symptoms: Central Sleep Apnea (CSA) represents a critical condition where breathing repeatedly stops and starts during sleep.
This condition differs from the more commonly known Obstructive Sleep Apnea by the fact that it involves the central nervous system.
This article delves into the symptoms and causes of CSA, providing comprehensive insights into understanding and identifying this condition.
What is Central Sleep Apnea?
Central Sleep Apnea (CSA) is a type of sleep disorder characterized by pauses in breathing during sleep. Unlike common breathing interruptions, CSA occurs not because of a physical blockage in the airway, but due to the brain’s failure to signal the muscles responsible for controlling breathing. This condition can affect anyone, but it is more prevalent in individuals with certain medical conditions or those at an advanced age.
Central Sleep Apnea is distinguished by its unique cause: the brain’s inconsistent signals that manage breathing. During sleep, individuals with CSA may experience a cessation of respiratory effort, meaning they make no effort to breathe for brief periods. These interruptions can lead to fragmented sleep, reduced oxygen levels in the blood, and, consequently, may not provide the restorative benefits that quality sleep usually offers.
How Central Sleep Apnea Differs from Obstructive Sleep Apnea
While Central Sleep Apnea and Obstructive Sleep Apnea (OSA) share the common symptom of pause in breathing during sleep, their causes are fundamentally different, leading to different treatment approaches.
Obstructive Sleep Apnea is far more common and occurs when the airway is physically blocked, often by the relaxation of throat muscles, which impedes the flow of air into the lungs during sleep. Individuals with OSA typically make efforts to breathe, but are unable to get enough air due to the blockage. This can result in loud snoring, gasping, or choking sounds as the person tries to breathe.
Central Sleep Apnea, on the other hand, is rooted in the central nervous system. It happens because the brain doesn’t send proper signals to the muscles that control breathing. This means that, in CSA, there may be no effort to breathe for short periods, leading to silent interruptions in breathing. Unlike OSA, snoring is not a typical symptom of CSA.
The differentiation between CSA and OSA is crucial for effective treatment. OSA treatments often focus on physically keeping the airway open during sleep, using devices such as Continuous Positive Airway Pressure (CPAP) machines or dental appliances. In contrast, CSA treatments may involve addressing the underlying medical conditions that affect the brain’s ability to control breathing, or using adaptive servo-ventilation (ASV), a device that helps regulate breathing patterns.
Understanding these distinctions is essential for proper diagnosis and management of sleep apnea. If you suspect you have sleep apnea, it’s important to consult with a healthcare provider who can recommend the appropriate tests and treatments based on the type of sleep apnea you might have.
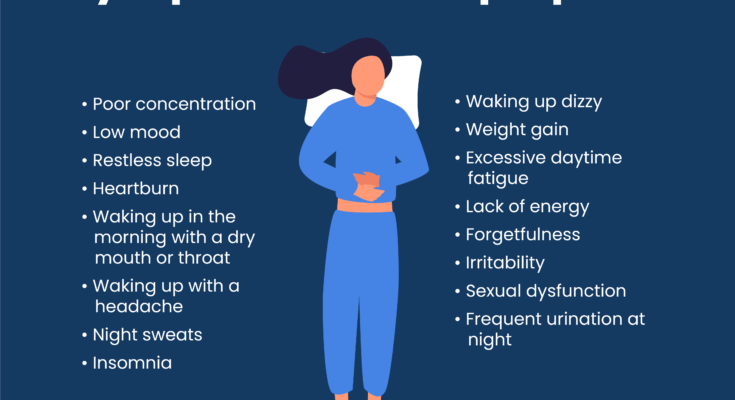
Symptoms of Central Sleep Apnea
Recognizing the symptoms of CSA is crucial for early diagnosis and treatment. Here’s a comprehensive guide to the common symptoms of Central Sleep Apnea.
1. Intermittent Pauses in Breathing
One of the hallmark symptoms of CSA is the noticeable, intermittent pauses in breathing while asleep. These pauses can last from a few seconds to minutes and may occur multiple times per hour. They are often identified by a bed partner rather than the person suffering from CSA.
2. Chronic Fatigue and Daytime Sleepiness
Due to the disrupted sleep patterns caused by breathing pauses, individuals with CSA often experience chronic fatigue and excessive daytime sleepiness. This can affect concentration, productivity, and the overall quality of life.
3. Abrupt Awakenings with Shortness of Breath
People with Central Sleep Apnea may wake up abruptly, gasping or choking for air. These awakenings are the body’s emergency response to resume breathing and can significantly disrupt sleep continuity.
4. Difficulty Staying Asleep (Insomnia)
Difficulty maintaining sleep, or insomnia, is a common symptom among those with CSA. Individuals may find it hard to stay asleep due to the frequent awakenings caused by breathing interruptions.
5. Morning Headaches
Morning headaches are a frequent complaint among individuals with CSA. These headaches are often due to the lack of oxygen and fragmented sleep patterns experienced throughout the night.
6. Cognitive Impairment
Cognitive functions, such as memory and attention, can be negatively affected in individuals with CSA. This is attributed to the poor sleep quality and oxygen deprivation associated with the condition.
7. Mood Changes
Mood disturbances, including irritability and depression, can also be symptoms of CSA. The chronic lack of restful sleep can take a toll on emotional well-being.
8. Snoring
While snoring is more commonly associated with Obstructive Sleep Apnea (OSA), some individuals with CSA may also snore. However, it’s important to note that snoring is not as predominant in CSA as it is in OSA.
9. Heart Problems
Central Sleep Apnea can be linked to heart conditions, such as atrial fibrillation or congestive heart failure. Individuals with heart issues may have a higher risk of developing CSA.
Causes of Central Sleep Apnea
Understanding the causes of Central Sleep Apnea is crucial for identifying risk factors and exploring effective treatments. This condition can be complex, influenced by various factors that may vary from person to person.
1. Heart Conditions
Heart-related problems, especially congestive heart failure, are closely linked with Central Sleep Apnea. Heart issues can affect the body’s ability to regulate breathing while sleeping.
2. Stroke or Brain Infection
A stroke or any form of brain infection can impair the brain’s ability to manage the breathing process. Damage to the brainstem, which controls breathing, can lead to CSA.
3. Use of Opioid Medications
Opioids, particularly long-acting ones, can disrupt the normal respiratory drive. People using opioid medications may experience irregular breathing patterns that lead to CSA.
4. Altitude Changes
Sudden changes in altitude can affect the body’s breathing patterns. High altitudes can trigger CSA in some individuals due to the decreased oxygen levels and altered breathing control.
5. Neurological Conditions
Certain neurological conditions, such as Parkinson’s disease or ALS (Amyotrophic Lateral Sclerosis), can interfere with the brain’s ability to send signals to the breathing muscles, leading to CSA.
6. Cheyne-Stokes Breathing
This specific pattern of breathing, characterized by gradual increases and decreases in breathing effort and air flow, is often associated with Central Sleep Apnea. It’s commonly seen in patients with heart failure or stroke.
Risk Factors for Central Sleep Apnea
Understanding the risk factors associated with CSA is crucial for identifying those who are most vulnerable to this condition. These risk factors can be broadly categorized into age, gender, and underlying health conditions.
Age
Age plays a significant role in the risk of developing Central Sleep Apnea. The disorder is more commonly observed in older adults, particularly those over the age of 65. As the body ages, changes in brain function and sleep patterns may increase the likelihood of CSA. Older adults are more prone to medical conditions that can lead to CSA, making age a prominent risk factor for the disorder.
Gender
Gender is another critical determinant in the risk of developing CSA. Research indicates that men are at a higher risk compared to women for experiencing Central Sleep Apnea. The reasons behind this gender disparity are not entirely clear but may be related to differences in body fat distribution, hormonal variations, and the structure of the airway, which can influence breathing patterns during sleep.
Underlying Health Conditions
Several underlying health conditions significantly increase the risk of Central Sleep Apnea. These include:
- Heart Disorders: Individuals with atrial fibrillation or congestive heart failure are at an elevated risk of CSA due to the impact of these conditions on the body’s ability to regulate breathing during sleep.
- Neurological Diseases: Conditions affecting the brainstem or the central nervous system, such as Parkinson’s disease or stroke, can disrupt the brain’s ability to control breathing, leading to CSA.
- High Altitude Exposure: Temporary exposure to high altitudes can trigger CSA in some individuals due to the lower oxygen levels, which can affect breathing patterns during sleep.
- Use of Opioids: Long-term use of opioid medications can alter the brain’s respiratory control mechanisms, increasing the risk of CSA.
- Obesity: While more commonly associated with Obstructive Sleep Apnea, obesity can also increase the risk of CSA, particularly when associated with other underlying health conditions.
Understanding these risk factors is essential for individuals and healthcare providers to identify those at increased risk for Central Sleep Apnea. Early recognition and intervention can significantly improve treatment outcomes and enhance the quality of life for those affected by CSA. If you believe you or someone you know is at risk for CSA, consulting with a healthcare provider for a comprehensive evaluation is strongly recommended.
Complications of Untreated Central Sleep Apnea
Untreated central sleep apnea (CSA) can lead to a range of complications that affect various aspects of health and quality of life. Understanding these potential risks is essential for recognizing the importance of seeking treatment. Below, we explore the major complications associated with untreated CSA, including cardiovascular issues, daytime fatigue and its impact on daily life, and mental health concerns.
Cardiovascular Issues
Central sleep apnea is closely linked to cardiovascular problems, a connection that underscores the critical nature of this sleep disorder. Individuals with untreated CSA are at a higher risk for conditions such as heart failure, atrial fibrillation (an irregular heart rhythm), stroke, and hypertension (high blood pressure). The repetitive stopping and starting of breathing during sleep can lead to decreased oxygen levels and increased carbon dioxide levels in the blood, which can strain the heart and vascular system. Over time, this strain can contribute to the development or worsening of cardiovascular diseases, highlighting the importance of managing CSA to protect heart health.
Daytime Fatigue and Its Impact on Daily Life
Daytime fatigue is another significant complication of untreated central sleep apnea. This fatigue results from the disrupted sleep patterns and reduced oxygen levels associated with CSA, leading to excessive daytime sleepiness, decreased energy levels, and an overall feeling of being unrefreshed upon waking. The impact of this fatigue extends into various aspects of daily life, affecting concentration, productivity, and the ability to perform tasks that require alertness. It can also increase the risk of accidents or injuries, particularly for those who drive or operate heavy machinery. The pervasive nature of this fatigue often leads to a diminished quality of life, emphasizing the need for effective treatment strategies to alleviate these symptoms.
Mental Health Concerns
The link between untreated central sleep apnea and mental health concerns is well-documented. The chronic sleep disruption and resulting fatigue can contribute to a range of psychological issues, including depression, anxiety, and mood swings. The constant struggle to achieve restful sleep can lead to feelings of frustration, irritability, and a decreased sense of well-being. Moreover, the stress of dealing with a chronic condition like CSA can exacerbate mental health symptoms, creating a cycle that can be difficult to break without appropriate intervention. Addressing CSA through comprehensive treatment approaches can help mitigate these mental health concerns, improving overall emotional and psychological health.
The complications of untreated central sleep apnea—ranging from cardiovascular issues to daytime fatigue and mental health concerns—underscore the critical importance of timely diagnosis and treatment. Recognizing the symptoms of CSA and seeking professional medical advice can help prevent these potentially severe health consequences, improving both life expectancy and quality of life. If you suspect you or a loved one may be experiencing symptoms of central sleep apnea, it is crucial to consult with a healthcare provider to explore treatment options that can mitigate these risks.
Diagnosis of Central Sleep Apnea
Diagnosing CSA is crucial for managing its symptoms and preventing potential health complications. The diagnosis involves a combination of medical history review, physical examination, and specialized tests. Here’s a closer look at these components:
Medical History and Physical Examination
The first step in diagnosing Central Sleep Apnea involves a detailed review of the patient’s medical history and a physical examination. During this phase, healthcare providers look for any underlying conditions that might be contributing to the sleep apnea, such as heart or neuromuscular disorders. Patients are often asked about their sleep patterns, daytime sleepiness, and any instances of waking up gasping for air. Additionally, the physical examination may reveal signs that indicate sleep apnea, such as increased neck circumference or high blood pressure.
Sleep Studies and Other Diagnostic Tests
Following the initial evaluation, sleep studies, also known as polysomnography, are typically recommended. These studies are conducted overnight in a sleep lab, where various bodily functions during sleep are monitored, including brain activity, eye movements, heart rate, blood oxygen levels, and breathing patterns. For diagnosing Central Sleep Apnea specifically, attention is given to the respiratory patterns and the lack of effort in breathing rather than blockage of the airway.
In some cases, additional tests might be required to further investigate the causes of CSA or to rule out other conditions. These can include:
- Echocardiogram: An ultrasound of the heart to check for heart failure or other heart-related conditions that could be causing or contributing to CSA.
- MRI or CT scans: Imaging tests to examine the brain and other structures for abnormalities that might interfere with the brain’s ability to regulate breathing.
- Blood tests: To check for levels of certain chemicals and hormones that can affect breathing and sleep patterns.
The comprehensive approach to diagnosing Central Sleep Apnea through medical history, physical examination, and sleep studies ensures a thorough evaluation. This enables healthcare providers to tailor treatment strategies that address not only the symptoms of CSA but also any underlying conditions contributing to the disorder. If you suspect you might have Central Sleep Apnea, it’s essential to consult with a healthcare provider to get a proper diagnosis and treatment plan.
Treatment Options for Central Sleep Apnea
Understanding the available treatment options can significantly improve the quality of life for those affected by this condition. This article explores lifestyle changes, home remedies, breathing devices, medications, and surgical options tailored for CSA management.
Lifestyle Changes and Home Remedies
Lifestyle modifications play a crucial role in managing central sleep apnea. These changes can significantly reduce symptoms and improve sleep quality:
- Weight Management: Maintaining a healthy weight can alleviate symptoms of CSA. Excess weight can exacerbate breathing problems during sleep.
- Avoid Alcohol and Sleeping Pills: These substances can relax the muscles in your throat, interfering with the brain’s signals to breathe.
- Side Sleeping: Sleeping on your side instead of your back can help keep your airway open, reducing the risk of breathing pauses.
- Regular Sleep Schedule: Establishing a consistent sleep routine can help regulate your sleep pattern and improve the quality of your sleep.
Continuous Positive Airway Pressure (CPAP) and Other Breathing Devices
CPAP is the most commonly prescribed treatment for sleep apnea disorders, including CSA. This device works by delivering a steady stream of air through a mask to keep your airways open during sleep. For individuals with CSA, CPAP can help regulate breathing by ensuring continuous airflow, preventing the airway from collapsing or becoming blocked.
Other breathing devices, such as BiPAP (Bilevel Positive Airway Pressure) or ASV (Adaptive Servo-Ventilation), may be recommended for those who find CPAP uncomfortable or ineffective. These devices adjust the pressure based on your breathing patterns, providing a more customized treatment approach.
Medications and Surgery (In Specific Cases)
In some cases, medications may be prescribed to treat underlying conditions contributing to CSA, such as heart failure or neuromuscular disorders. It’s important to address these health issues to effectively manage sleep apnea symptoms.
Surgery may be considered as a last resort, particularly if other treatments have failed and there’s a clear anatomical reason for the CSA. Surgical options vary based on the underlying cause and may include procedures to correct abnormalities in the heart or nerves that affect breathing.
The choice of treatment for central sleep apnea depends on the severity of the condition and the presence of other underlying health issues. A healthcare professional can provide a comprehensive evaluation and recommend the most appropriate treatment plan tailored to individual needs. It’s crucial to follow the treatment plan closely and maintain regular follow-ups to ensure the best possible outcomes in managing CSA.
Preventive Measures for Central Sleep Apnea
Central Sleep Apnea (CSA) is a disorder where your breathing repeatedly stops and starts during sleep due to the brain’s failure to send proper signals to the muscles that control breathing. Unlike Obstructive Sleep Apnea, which is caused by a blockage in the airway, CSA requires a different approach to prevention and management. Here are tips for reducing the risk of Central Sleep Apnea and the importance of regular medical check-ups for individuals at risk.
Tips for Reducing the Risk of Central Sleep Apnea
- Maintain a Healthy Lifestyle: A balanced diet and regular exercise can help manage conditions like obesity and heart problems, which are often linked to CSA. Incorporating physical activity into your daily routine can improve heart health and potentially reduce the severity of CSA.
- Control Heart Conditions: Since CSA can be associated with heart disorders, managing heart health is crucial. This includes monitoring blood pressure, cholesterol levels, and following treatments prescribed for heart conditions.
- Avoid Substance Abuse: Alcohol and certain medications, especially opioids, can increase the risk of CSA. Limiting alcohol consumption and using medications as prescribed can mitigate this risk.
- Optimize Sleeping Environment: Ensure your sleeping environment promotes healthy sleep patterns. This includes maintaining a comfortable room temperature, reducing noise and light, and establishing a regular sleep schedule.
- Consider a CPAP Machine: For some individuals, using a Continuous Positive Airway Pressure (CPAP) machine at night can help keep the airway open and prevent episodes of stopped breathing. While more commonly used for Obstructive Sleep Apnea, it may be beneficial for some cases of CSA as recommended by a healthcare provider.
Importance of Regular Medical Check-Ups for At-Risk Individuals
Regular medical check-ups play a pivotal role in the early detection and management of Central Sleep Apnea, especially for individuals with risk factors such as heart disease, high altitude exposure, or a history of stroke. During these check-ups, healthcare providers can:
- Monitor Existing Health Conditions: Regular monitoring of conditions that could contribute to CSA ensures that any necessary adjustments to treatment plans are made promptly.
- Evaluate Sleep Health: Healthcare providers can assess symptoms related to poor sleep quality or disturbances that might indicate CSA. Early identification leads to timely intervention.
- Adjust Medications: For individuals on medications that could affect breathing during sleep, doctors can adjust dosages or prescribe alternatives to reduce the risk of CSA.
- Provide Tailored Advice: Based on your health status and lifestyle, medical professionals can offer personalized recommendations for reducing the risk of CSA.
However, while Central Sleep Apnea requires careful management, adopting a healthy lifestyle, controlling associated health conditions, avoiding substances that can exacerbate the condition, and maintaining regular medical check-ups can significantly reduce the risk and impact of CSA. Early detection and intervention are key to managing this sleep disorder effectively.
Conclusion
It’s important to recognize the signs of CSA, such as episodes of no breathing, abrupt awakenings with shortness of breath, and chronic fatigue despite a full night’s sleep. If you or someone you know is exhibiting these symptoms, it’s imperative to seek professional medical advice. A healthcare provider can offer a comprehensive evaluation, which may include overnight monitoring in a sleep lab, to accurately diagnose the condition and recommend an effective treatment plan. Treatments can vary from lifestyle changes and use of breathing devices to medications and surgery, depending on the severity and underlying cause of CSA.
We encourage anyone who suspects they might be dealing with Central Sleep Apnea not to delay in consulting a medical professional. Early diagnosis and treatment are key to managing the symptoms, improving sleep quality, and preventing further health complications. Remember, prioritizing your sleep health is a critical step towards maintaining overall well-being.
In summary, while Central Sleep Apnea can be a daunting condition, understanding its symptoms and seeking prompt medical advice can lead to effective management and a healthier, more restful night’s sleep. Take action today if you’re concerned about CSA – your health and well-being are worth it.