Cellulitis Symptoms: Cellulitis is a common, potentially serious bacterial skin infection. The condition typically presents as a swollen, red area of skin that feels hot and tender, and it can spread rapidly if not treated promptly.
Understanding the symptoms and causes of cellulitis is crucial for early detection and effective treatment. This comprehensive guide explores the key aspects of cellulitis, including its symptoms, underlying causes, risk factors, and prevention strategies.
What is Cellulitis?
Cellulitis is a common, potentially serious bacterial skin infection. The affected skin appears swollen, red, and is typically painful and warm to the touch. Cellulitis usually affects the skin on the lower legs, but it can occur on any part of the body. The infection can spread rapidly, making prompt treatment crucial to prevent more severe complications.
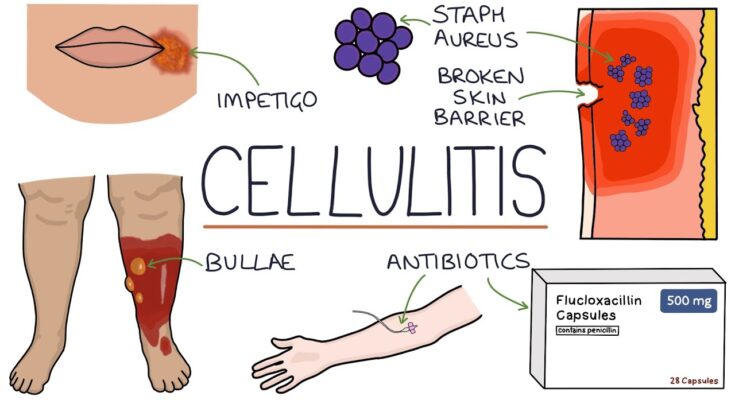
Unlike other skin infections, cellulitis penetrates deeper, affecting not just the surface of the skin but also the tissues beneath. This distinguishes it from conditions like impetigo, which is a more superficial infection involving the upper layers of the skin, and from dermatitis, which is inflammation of the skin without a bacterial cause. Furthermore, cellulitis does not form a head or pus-filled blisters that are characteristic of infections such as boils or abscesses. Its deeper involvement necessitates a different treatment approach, often involving oral or intravenous antibiotics to fight the infection effectively.
Prompt medical attention for cellulitis is vital to prevent the spread of the infection to the bloodstream or lymphatic system, which can lead to life-threatening complications. Recognizing the symptoms early and understanding how cellulitis differs from other skin infections can lead to quicker diagnosis and treatment, reducing the risk of complications.
Causes of Cellulitis: An In-Depth Guide
Cellulitis is a common, yet potentially serious bacterial skin infection. The condition typically results from bacteria entering through a break in the skin, leading to an infection that can spread rapidly if left untreated. Understanding the causes and risk factors associated with cellulitis is crucial for prevention and timely treatment. This guide will provide a comprehensive overview of how cellulitis occurs, the bacteria responsible, risk factors, and the pivotal role of skin breaks in fostering infection.
Overview of How Cellulitis Occurs
Cellulitis predominantly occurs when bacteria, most commonly Streptococcus and Staphylococcus, penetrate through a crack or break in your skin. Although these bacteria are often present on the skin without causing harm, they can lead to an infection if they bypass the skin’s protective barrier. This infection causes redness, swelling, warmth, and pain in the affected area. It’s a condition that can affect any part of the body, though it most frequently affects the skin on the lower legs.
Bacteria Responsible for Cellulitis
The two primary bacteria responsible for cellulitis are:
- Streptococcus: Known for causing a wide range of infections, from throat infections to more severe conditions like pneumonia.
- Staphylococcus: Particularly the strain known as methicillin-resistant Staphylococcus aureus (MRSA), can cause skin infections that are difficult to treat due to antibiotic resistance.
Occasionally, other bacteria or even fungi can cause cellulitis, especially in individuals with specific health conditions or those with weakened immune systems.
Risk Factors for Developing Cellulitis
Several factors can increase your likelihood of developing cellulitis, including:
- Skin Injuries: Cuts, fractures, burns, or insect bites provide gateways for bacteria to enter the skin.
- Skin Conditions: Eczema, athlete’s foot, and other conditions that break the skin can make you more susceptible.
- Chronic Conditions: Diabetes, obesity, and lymphedema can compromise the skin’s integrity, increasing infection risks.
- Weakened Immune System: Conditions or treatments that suppress the immune system, such as chemotherapy, increase susceptibility to cellulitis.
Understanding these risk factors is key to taking preventive measures, such as proper wound care and skin hygiene, to reduce the chances of developing cellulitis.
The Role of Skin Breaks in Leading to Infection
Breaks in the skin are the primary gateway for bacteria to cause cellulitis. Even minor disruptions in the skin’s surface can be enough for bacteria to enter and multiply, leading to infection. This underscores the importance of caring for even small wounds properly, keeping the skin clean, and moisturized to maintain its protective barrier.
However, cellulitis is a bacterial infection that arises from bacteria entering through breaks in the skin. Knowing the causes, responsible bacteria, risk factors, and how skin breaks lead to infection can aid in prevention and early detection, crucial steps in effectively managing and treating cellulitis. Regular skin checks, proper hygiene, and prompt attention to wounds are fundamental in reducing the risk of this potentially severe condition.
Symptoms of Cellulitis
Recognizing the early signs and symptoms of cellulitis is crucial for timely treatment and to prevent the infection from worsening. This article provides a detailed description of cellulitis symptoms, emphasizing early signs, and explains how symptoms can progress if the infection is not treated.
Early Signs of Cellulitis:
- Redness: One of the first signs of cellulitis is an area of skin that becomes red. This redness often expands over time.
- Swelling: The affected area may feel swollen and can rise slightly due to inflammation.
- Warmth: When touching the infected area, it feels warmer than surrounding areas.
- Pain: The area is often tender or painful to touch.
- Skin Tightness: The skin over the affected area may feel tighter than usual.
Progression of Symptoms:
Without appropriate treatment, cellulitis symptoms can quickly progress, leading to more severe health issues. Here’s what might happen if cellulitis is left untreated:
- Spreading of the Infection: The red and swollen area can increase in size as the infection spreads.
- Fever: You may develop a fever as your body tries to fight off the infection.
- Chills and Sweats: Along with fever, chills and sweats are common.
- Feeling Unwell: A general feeling of being unwell, fatigue, or dizziness can occur.
- Blisters: In more severe cases, blisters may form on the infected skin.
- Red Streaks: You might notice red streaks spreading from the original infection site, indicating the bacteria are moving through the lymphatic system.
Visuals for Quick Symptom Identification:
For quick identification of cellulitis, look for:
- Red, Swollen Skin: A visual cue of cellulitis is a distinct area of redness and swelling.
- Warmth and Pain: If the area feels warmer than surrounding skin and is painful, it could be a sign of cellulitis.
Bullet Points for Symptom Checklist:
- Red, swollen area on the skin
- Warmth over the affected area
- Pain or tenderness
- Skin tightness or shininess
- Fever (in advanced cases)
- Chills and sweats
- Blisters or red streaks (in severe cases)
Early identification and treatment of cellulitis are key to preventing the spread of infection and avoiding severe complications. If you suspect you have cellulitis, seek medical attention promptly to receive the necessary treatment.
Complications of Untreated Cellulitis
Cellulitis, a common yet potentially serious bacterial skin infection, requires immediate medical attention to prevent severe complications. When left untreated, cellulitis can lead to life-threatening conditions, underscoring the importance of recognizing its symptoms early and consulting healthcare professionals for proper diagnosis and treatment.
Potential Complications
The most alarming complication of untreated cellulitis is the progression to sepsis, a systemic infection that occurs when bacteria from the infected area enter the bloodstream. Sepsis is a medical emergency characterized by body-wide inflammation, leading to organ failure and, in severe cases, death. This drastic outcome highlights the critical need for early intervention in cases of cellulitis.
Besides sepsis, untreated cellulitis can also result in the following complications:
- Abscess formation: Pockets of pus that require surgical drainage.
- Lymphangitis: Infection of the lymph channels, causing inflammation and potentially affecting the immune system’s functionality.
- Necrotizing fasciitis: A rare but severe infection that causes tissue death; often referred to as “flesh-eating disease.”
- Chronic swelling: Persistent swelling of the affected limb due to damage to the lymphatic system.
The Importance of Seeking Medical Advice
Early and effective treatment of cellulitis is crucial to prevent these severe complications. If you suspect you have cellulitis—indicated by red, swollen, warm, and painful skin—seek medical advice promptly. Healthcare providers can offer accurate diagnoses and tailor treatments, typically involving antibiotics to combat the bacterial infection.
Timely medical intervention not only facilitates a faster recovery but also minimizes the risk of complications, safeguarding your health and well-being. Ignoring symptoms or delaying treatment increases the risk of severe outcomes, making it paramount to act quickly when signs of cellulitis appear.
However, understanding the potential complications of untreated cellulitis underscores the importance of seeking medical advice at the first sign of infection. By doing so, individuals can ensure the best possible outcome, preventing the progression of the disease and the onset of life-threatening complications.
Diagnosing Cellulitis: A Comprehensive Guide
Proper diagnosis is crucial for effective treatment. Here’s a closer look at the diagnosis process and how healthcare professionals distinguish cellulitis from conditions that mimic its symptoms.
Diagnosis Process for Cellulitis
- Medical History and Physical Examination: The first step involves a detailed discussion of your medical history and a thorough physical exam. Doctors look for signs of infection, such as redness, swelling, warmth, and pain in the affected area.
- Blood Tests: While not always necessary, blood tests may be conducted to check for the presence of bacteria and to assess your overall health, including checking for signs of infection in your blood.
- Imaging Tests: In certain cases, particularly if the doctor suspects that the infection has spread deeper beneath the skin or wants to rule out other conditions, imaging tests like X-rays, ultrasounds, or MRIs might be recommended.
- Wound Culture: If there’s an open wound or pus, a sample might be taken and sent to a lab to identify the bacteria causing the infection. This step is especially important if you’ve had recurrent episodes of cellulitis or if the infection isn’t responding to standard treatment.
Differentiating Cellulitis from Similar Conditions
Cellulitis often presents symptoms that are similar to other conditions, making it a challenge to diagnose. Here’s how doctors differentiate it:
- Erysipelas: This infection also involves the upper layers of the skin but typically has a more distinct border between the infected and healthy skin. Erysipelas causes more pronounced swelling and is usually caused by a specific type of bacteria.
- Deep Vein Thrombosis (DVT): DVT is a blood clot in a deep vein, often in the legs, which can mimic cellulitis due to similar swelling and redness. Doctors may use ultrasound to look for clots.
- Dermatitis: Dermatitis is an inflammation of the skin that can cause redness, itching, and swelling. Unlike cellulitis, it’s often accompanied by a history of allergies or asthma and does not typically involve fever or a rapid spread of symptoms.
- Gout: Gout can cause redness, swelling, and pain in the joints, which may resemble cellulitis. However, gout attacks are more likely to affect the big toe, and the diagnosis is supported by the presence of uric acid crystals in joint fluid.
- Necrotizing Fasciitis: This is a severe, life-threatening infection that spreads rapidly. It requires immediate medical attention. Unlike cellulitis, which progresses more slowly, necrotizing fasciitis causes severe pain, systemic symptoms, and, potentially, toxic shock.
For accurate diagnosis and treatment, always consult a healthcare professional if you suspect you have cellulitis or any similar condition. Early intervention is key to preventing complications and ensuring a swift recovery.
This guide aims to provide a clear understanding of how cellulitis is diagnosed and differentiated from other conditions. Armed with this knowledge, you can seek timely medical advice and treatment, leading to better health outcomes.
Treatment Options for Cellulitis: A Comprehensive Guide
Prompt treatment is crucial to prevent the infection from spreading throughout your body. This article delves into the effective treatment options for cellulitis, highlighting the central role of antibiotics, the potential need for hospitalization in severe cases, and the supportive role of home care in the recovery process.
Antibiotics: The First Line of Defense
The primary treatment for cellulitis is antibiotics. These medications are effective in killing the bacteria responsible for the infection. Antibiotics can be administered orally or, in more severe cases, intravenously. The choice of antibiotics and the duration of treatment depend on the severity of the infection and the specific bacteria causing it. Patients typically notice an improvement within a few days of starting antibiotics, but it’s crucial to complete the entire course prescribed by your healthcare provider to fully eradicate the infection and prevent recurrence.
Hospitalization for Severe Cases
While most cases of cellulitis can be successfully treated at home with oral antibiotics, severe cases may require hospitalization. Indications for hospital admission include a rapid spread of the infection, signs of systemic illness (such as fever, chills, and malaise), and underlying conditions that complicate cellulitis (like diabetes or weakened immune systems). In the hospital, patients may receive intravenous antibiotics and other supportive care to manage symptoms and monitor the infection’s progression closely.
The Role of Home Care in Supporting Recovery
Home care plays a vital role in supporting the recovery process from cellulitis. Key elements of effective home care include:
- Rest: Keeping the affected area elevated can help reduce swelling and pain.
- Hygiene: Maintaining cleanliness of the infected area is essential to prevent further spread of the infection.
- Monitoring: Watching for signs of worsening symptoms or the spread of infection is critical. If the area of redness expands or symptoms do not improve after starting antibiotics, it’s important to contact your healthcare provider.
- Completing Antibiotic Course: Adherence to the antibiotic regimen, even after symptoms improve, ensures the infection is fully resolved.
Effective treatment of cellulitis involves a combination of antibiotics, potential hospitalization for severe cases, and supportive home care measures. Early diagnosis and treatment are essential to prevent the spread of the infection and ensure a full recovery. If you suspect you have cellulitis, consult your healthcare provider immediately to discuss the best treatment approach for your specific situation.
Preventing Cellulitis: Essential Tips and Advice
Cellulitis is a common, potentially serious bacterial skin infection. The key to managing cellulitis lies in prevention, especially for individuals with a history of the condition or those at higher risk. Here are practical tips to help prevent cellulitis, ensuring your skin remains healthy and infection-free.
1. Maintain Good Hygiene
Keeping your skin clean is the first step in preventing cellulitis. Wash regularly with soap and water, especially after cuts or wounds. This simple practice can significantly reduce the risk of bacteria entering and infecting the skin.
2. Treat Wounds Promptly and Properly
Even minor injuries like scratches or insect bites can become entry points for bacteria. Clean wounds immediately with water and apply an antiseptic. Cover with a sterile bandage to protect against infection. Change bandages daily or whenever they become wet or dirty.
3. Moisturize Your Skin
Dry, cracked skin can make it easier for bacteria to breach your skin’s protective barrier. Regularly applying moisturizer helps keep your skin hydrated and intact, reducing the infection risk.
4. Wear Protective Gear
If you’re involved in activities that may cause skin injuries, such as gardening or sports, wear appropriate protective clothing. Gloves, long sleeves, and pants can shield your skin from scrapes and cuts, minimizing the chances of cellulitis.
5. Manage Chronic Conditions
Conditions like diabetes or circulation problems can increase your risk of cellulitis. Manage these conditions effectively through regular medical check-ups, medication, and lifestyle changes. Healthy blood sugar levels and improved circulation can strengthen your body’s defense against infections.
6. Avoid Tight Clothing
Tight, restrictive clothing can cause skin chafing, leading to breaks in the skin. Opt for loose-fitting, breathable fabrics to prevent skin damage and reduce the risk of cellulitis.
7. Elevate Swollen Limbs
For those with a history of cellulitis or at higher risk, elevating swollen limbs can improve circulation and reduce swelling. Better circulation can help prevent infections by allowing your immune system to function more effectively.
By incorporating these tips into your daily routine, you can significantly reduce your risk of developing cellulitis. Remember, if you notice signs of infection, such as redness, swelling, warmth, or fever, seek medical attention promptly. Early treatment is crucial to prevent the spread of infection and ensure a quick recovery.
When to See a Doctor for Cellulitis
Cellulitis is a common, potentially serious bacterial skin infection. The affected skin appears swollen, red, and is usually painful and warm to the touch. While mild cases can sometimes be managed at home, it’s crucial to know when to seek professional medical advice. This guide will help you recognize the signs that warrant a doctor’s visit and set your expectations for the consultation.
Recognizing Signs That Warrant a Doctor’s Visit
Immediate medical attention for cellulitis is essential to prevent the infection from spreading and to avoid serious complications. Here are key signs that you should see a doctor:
- Increasing Swelling or Redness: If the area of redness and swelling is expanding, it’s a clear sign that the infection is not under control.
- Fever: Experiencing a fever indicates that your body is fighting a significant infection.
- Pain Intensification: An increase in pain can suggest the infection is worsening.
- Presence of Red Streaks: Red streaks leading away from the infected area toward your heart are a sign of lymphangitis, a condition that needs prompt medical intervention.
- Feeling Unwell: Symptoms such as dizziness, fatigue, or a general feeling of illness are indicators that the infection might be spreading.
What to Expect During the Consultation
Knowing what to expect during your doctor’s visit can help alleviate some of the stress associated with seeking medical care for cellulitis. Here’s what typically happens:
- Medical History and Symptoms Review: Your doctor will ask about your symptoms, their onset, and any pre-existing health conditions that might affect your treatment plan.
- Physical Examination: The doctor will examine the affected skin to assess the severity of the infection.
- Treatment Plan Discussion: If cellulitis is diagnosed, your doctor will outline a treatment plan, which usually involves antibiotics to fight the infection. They will explain the importance of completing the entire course of antibiotics and may schedule follow-up visits to monitor your progress.
- Home Care Instructions: You’ll receive advice on how to care for the infected area at home, such as elevating the affected limb to reduce swelling and applying cool, damp cloths to relieve discomfort.
- Warning Signs: Before you leave, your doctor will inform you about signs of complications or infection worsening, which would require immediate medical attention.
Prompt treatment of cellulitis is crucial to prevent the spread of infection and avoid serious health complications. By recognizing the signs that necessitate a doctor’s visit and understanding what to expect during the consultation, you can take an active role in your healthcare and recovery process.
FAQ Section on Cellulitis: Symptoms and Causes
1. What is cellulitis?
Cellulitis is a common, potentially serious bacterial skin infection. It appears as a swollen, red area that is hot and tender to the touch and may spread rapidly. Skin on any part of the body can be affected, but the condition most often affects the skin on the legs.
2. What causes cellulitis?
Cellulitis is caused by bacteria, most commonly streptococcus and staphylococcus, entering through a crack or break in your skin. Cuts, insect bites, burns, surgical wounds, or even dry, flaky skin can open the door for these bacteria to enter the body.
3. What are the symptoms of cellulitis?
The symptoms include redness, swelling, tenderness, pain in the affected area, a warm feeling over the affected skin, fever, and in severe cases, blisters or red streaks. If you experience these symptoms, especially if you have a fever, seek medical attention promptly.
4. Can cellulitis spread to other parts of the body?
Yes, without proper treatment, the infection can spread to the lymph nodes and bloodstream, becoming life-threatening. Early treatment with antibiotics is crucial to prevent the spread of infection.
5. How can I prevent cellulitis?
Preventive measures include proper wound care, keeping the skin moisturized, promptly treating any skin conditions like eczema or athlete’s foot, and protecting the skin from cuts and abrasions. If you have a wound, keep it clean and covered to prevent infection.
6. Is cellulitis contagious?
Cellulitis is not contagious. It cannot spread from person to person through close contact. However, the bacteria causing cellulitis can be transmitted, though the transmission does not necessarily result in cellulitis in the other person.
7. Who is at risk for cellulitis?
While anyone can develop cellulitis, individuals with a weakened immune system, diabetes, lymphedema, or skin conditions like eczema are at higher risk. Breaks in the skin, poor circulation, and previous episodes of cellulitis also increase the risk.
8. When should I see a doctor for cellulitis?
You should see a doctor if you notice areas of red, swollen, and tender skin, especially if the area starts to expand or is accompanied by fever. Early treatment is key to preventing complications.
Conclusion
Taking preventive measures cannot be overstated. Simple practices like maintaining good hygiene, promptly treating wounds, and keeping the skin moisturized can significantly reduce the risk of developing cellulitis. Moreover, individuals with a history of cellulitis or those at higher risk should be particularly vigilant and consider consulting healthcare professionals for personalized advice on prevention strategies.
Early treatment is key to managing cellulitis effectively. At the first sign of symptoms, seeking medical advice is paramount. Timely intervention with appropriate antibiotics can prevent the spread of the infection, alleviating symptoms swiftly and avoiding severe health issues.
In conclusion, understanding the symptoms and causes of cellulitis, coupled with proactive prevention and prompt treatment, is essential. It empowers individuals to take charge of their health, ensuring a swift return to well-being. Let this knowledge serve as a foundation for a healthier, more informed approach to managing and preventing cellulitis.