Congenital Diaphragmatic Hernia Treatment: Congenital Diaphragmatic Hernia (CDH) represents a significant challenge in neonatal medicine, involving a defect in the diaphragm that allows abdominal organs to move into the chest cavity, affecting lung development.
This comprehensive guide aims to elucidate the diagnosis and treatment modalities available for CDH, leveraging the latest research and clinical practices to offer insights for healthcare professionals, patients, and their families.
What is Congenital Diaphragmatic Hernia (CDH)?
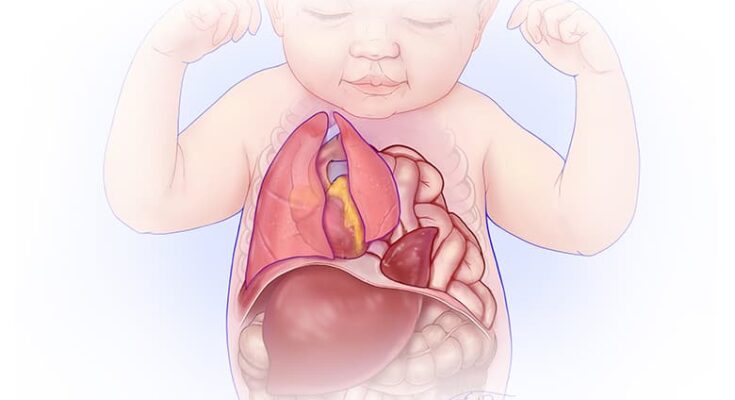
Congenital Diaphragmatic Hernia (CDH) is a serious medical condition that occurs when a baby is born with an opening in the diaphragm, the muscle that helps in breathing by separating the chest cavity from the abdominal cavity. This opening allows organs that are normally situated in the abdomen, such as the stomach, intestines, liver, or spleen, to move into the chest cavity. This abnormal positioning of organs can significantly affect a newborn’s lung development and function, leading to breathing difficulties after birth.
Causes and Risk Factors
The exact cause of Congenital Diaphragmatic Hernia is not fully understood, but it is believed to result from a combination of genetic and environmental factors. Here are some potential causes and risk factors associated with CDH:
- Genetic Factors: A history of CDH in the family increases the risk of the condition in newborns. Certain genetic conditions and chromosomal abnormalities may also be linked to the development of CDH.
- Environmental Factors: Some studies suggest that maternal smoking, drug use, or exposure to certain medications during pregnancy can increase the risk of CDH.
- Vitamin Deficiencies: Lack of certain vitamins in a mother’s diet during pregnancy, like folic acid, might contribute to the development of CDH in the fetus.
- Multiple Pregnancies: Babies born as part of multiple pregnancies (twins, triplets, etc.) may have a higher risk of CDH.
How CDH Affects Breathing and Development in Newborns
CDH significantly impacts the breathing and overall development of newborns due to the displacement of abdominal organs into the chest cavity, which can lead to several complications:
- Reduced Lung Space: The presence of abdominal organs in the chest limits the space available for the lungs to expand, leading to underdeveloped (hypoplastic) lungs.
- Pulmonary Hypertension: CDH can cause high blood pressure in the lungs (pulmonary hypertension), making it difficult for oxygen to enter the bloodstream and causing further breathing difficulties.
- Respiratory Distress: Newborns with CDH often suffer from respiratory distress immediately after birth, which can manifest as rapid breathing, grunting, or a bluish skin color due to lack of oxygen.
- Long-term Health Issues: Children who survive CDH may face long-term health issues, including chronic lung disease, gastrointestinal problems, and developmental delays.
However, Congenital Diaphragmatic Hernia is a life-threatening condition that requires immediate medical attention. Understanding the causes and risk factors associated with CDH can help in early diagnosis and treatment, improving the outcomes for affected newborns. Advances in prenatal diagnosis and neonatal care have significantly improved the survival rates and quality of life for babies with CDH, highlighting the importance of specialized medical care for these patients.
Signs and Symptoms of Congenital Diaphragmatic Hernia (CDH)
Early detection and immediate medical intervention are crucial for the health and survival of infants with CDH. Below, we explore the early indicators of CDH in infants and explain why these symptoms necessitate urgent medical attention.
Early Indicators of CDH in Infants
CDH can present a range of signs and symptoms shortly after birth, which are critical to recognize for early diagnosis and treatment. These include:
- Difficulty Breathing: One of the most immediate and noticeable signs of CDH is difficulty breathing. Infants may exhibit rapid breathing (tachypnea), flaring of the nostrils, or a bluish coloration of the skin (cyanosis) due to insufficient oxygen.
- Abnormal Chest Appearance: The chest may appear asymmetrical or bulging on one side due to the displacement of abdominal organs into the chest cavity.
- Diminished Breath Sounds: Upon examination, a healthcare provider may notice reduced or absent breath sounds on one side of the chest, indicating where the lung may be compressed or underdeveloped.
- A Concave or Flat Appearance of the Abdomen: As organs move into the chest cavity, the abdomen may appear unusually concave or flat, indicating the abnormal positioning of abdominal contents.
Why These Symptoms Necessitate Immediate Medical Attention
The symptoms of CDH are indicative of underlying issues that can significantly impact an infant’s ability to breathe and, consequently, their oxygenation and overall health. Here are the reasons why immediate medical attention is critical:
- Respiratory Distress: The primary concern with CDH is respiratory distress due to underdeveloped lungs (pulmonary hypoplasia) and the pressure exerted by the displaced organs on the lungs. Without prompt intervention, this can lead to life-threatening complications.
- Risk of Hypoxemia: Difficulty in breathing can lead to hypoxemia, a condition where there is a deficient level of oxygen in the blood. Hypoxemia can result in damage to vital organs, including the brain and heart, if not addressed swiftly.
- Need for Specialized Care: CDH requires a multidisciplinary approach for management, including surgical repair of the diaphragm and supportive measures to enhance lung development and function. Early intervention by specialists can improve the prognosis and quality of life for infants with CDH.
However, recognizing the early signs and symptoms of Congenital Diaphragmatic Hernia in infants is crucial for timely medical intervention. The complexity of CDH necessitates a prompt and coordinated approach to care, underscoring the importance of immediate medical attention to mitigate risks and support the healthy development of affected infants. Parents and caregivers should seek medical advice if they notice any signs of distress, abnormal breathing patterns, or unusual physical appearances in their newborns, as early diagnosis and treatment can significantly influence the outcomes for children with CDH.
Diagnosis of Congenital Diaphragmatic Hernia
Early and accurate diagnosis of CDH is crucial for planning appropriate treatment and improving outcomes. This section explores the various methods used for diagnosing CDH, focusing on prenatal screening, postnatal diagnostic techniques, physical examination findings, imaging tests, and other diagnostic procedures.
Prenatal Screening and Diagnosis Methods
Prenatal screening for CDH primarily involves ultrasound examinations, which are typically performed during the second trimester of pregnancy. High-resolution ultrasounds can detect the herniation of abdominal organs into the chest cavity, showing the position of the liver and the presence of bowel loops in the thoracic cavity. In some cases, fetal MRI (Magnetic Resonance Imaging) may also be used to provide a more detailed view of the fetus’s anatomy, helping in the diagnosis of CDH and planning for treatment after birth.
Postnatal Diagnostic Techniques
After birth, the diagnosis of CDH is confirmed through a combination of physical examinations and imaging tests. The initial indication of CDH in a newborn may include respiratory distress, a scaphoid abdomen (appearing hollow), and diminished breath sounds on the affected side.
Physical Examination Findings
Physical examination of an infant suspected to have CDH may reveal several key findings. These include rapid breathing (tachypnea), cyanosis (a bluish tint to the skin indicating low oxygen levels), and signs of difficulty breathing such as flaring nostrils or grunting. A scaphoid abdomen, where the abdominal cavity appears concave, can also be a significant indicator of CDH.
Imaging Tests: Ultrasound, MRI, and X-ray
Imaging tests play a pivotal role in diagnosing CDH and assessing the extent of the condition.
- Ultrasound: Besides its prenatal use, ultrasound can be helpful postnatally to examine the position of abdominal organs.
- MRI: Provides detailed images of the diaphragm, organs, and structures within the chest and abdomen. It is particularly useful in complex cases or when planning surgical intervention.
- X-ray: A chest X-ray is often the first imaging test performed after birth if CDH is suspected. It can quickly reveal the displacement of abdominal organs into the chest cavity, showing the position and condition of the lungs and heart.
Other Diagnostic Procedures
In addition to imaging tests, other diagnostic procedures may be employed to assess the baby’s condition and the severity of the hernia. These can include:
- Echocardiography: To evaluate the heart’s function and structure, as congenital heart defects may occur alongside CDH.
- Blood tests: To check for possible complications such as anemia or infection.
- Pulse oximetry: To measure the oxygen levels in the blood, providing crucial information about the baby’s respiratory status.
Early diagnosis of Congenital Diaphragmatic Hernia through these methods is essential for managing the condition effectively. It allows healthcare providers to assess the severity of the hernia, plan for necessary interventions, and offer the best possible prognosis for affected infants.
Treatment Options for Congenital Diaphragmatic Hernia (CDH)
Congenital Diaphragmatic Hernia (CDH) is a serious condition that requires timely and effective treatment to ensure the best outcomes for affected infants. Treatment options for CDH can be broadly categorized into surgical treatments, non-surgical management, and innovative approaches that are shaping the future of CDH care.
Surgical Treatment: Techniques and Timing
The cornerstone of CDH treatment is surgical repair of the hernia, which can be performed using various techniques based on the individual case and the severity of the condition. The primary goal of surgery is to reposition the abdominal organs into their correct place and repair the diaphragm to prevent reoccurrence.
- Minimally Invasive Surgery (MIS): This approach, including laparoscopy or thoracoscopy, is favored for its reduced recovery times and minimal scarring. MIS allows surgeons to repair the hernia through small incisions using specialized instruments and cameras.
- Open Repair: In more severe cases, an open surgical repair may be necessary. This traditional approach provides direct access to the affected area but comes with longer recovery periods and larger scars.
- Timing: The timing of surgery is critical and is typically determined by the infant’s stability, especially their ability to breathe independently and maintain stable blood circulation.
Non-surgical Treatment Options and Supportive Care
Before and after surgery, supportive care is essential for managing CDH and improving survival rates. Non-surgical interventions focus on stabilizing the infant and addressing complications.
- Respiratory Support: Given the high risk of lung hypoplasia and pulmonary hypertension in CDH patients, respiratory support, including mechanical ventilation and oxygen therapy, is crucial.
- Nutrition Management: Nutritional support is vital for growth and recovery, often requiring specialized feeding strategies to ensure adequate intake while minimizing risks.
Innovations in CDH Treatment: Recent Advancements and Future Directions
The treatment of CDH is continuously evolving, with research and innovation opening new avenues for care and improving prognoses.
- Fetal Interventions: Prenatal surgical techniques, such as fetoscopic endoluminal tracheal occlusion (FETO), are being explored to promote lung growth before birth, offering hope for severe cases.
- Regenerative Medicine: Advances in tissue engineering and regenerative medicine are paving the way for innovative treatments, such as the development of bioengineered diaphragm patches that could improve repair outcomes and function.
However, the treatment of Congenital Diaphragmatic Hernia encompasses a range of surgical and non-surgical strategies, each tailored to the individual needs of the infant. Continuous advancements in medical science are enhancing these treatment options, promising better outcomes and brighter futures for those affected by CDH.
Challenges in the Treatment of Congenital Diaphragmatic Hernia (CDH)
Treating Congenital Diaphragmatic Hernia (CDH) presents a unique set of challenges that healthcare providers must navigate carefully. CDH, a condition where a hole in the diaphragm allows abdominal organs to move into the chest, can severely impact a baby’s lung development and overall health. This article delves into the complications associated with CDH and its treatment, as well as the long-term outlook and potential developmental concerns for affected infants.
Complications Associated with CDH and Its Treatment
The treatment of CDH, often involving surgical repair of the diaphragm and supportive care for respiratory function, is complex and carries several risks. Complications can arise both from the condition itself and the interventions used to treat it. These include:
- Respiratory Distress: Due to underdeveloped lungs, infants with CDH are at a high risk of respiratory distress after birth. This is one of the most immediate and critical challenges to manage.
- Pulmonary Hypertension: Many babies with CDH develop pulmonary hypertension, a condition where high blood pressure in the lungs’ arteries puts extra strain on the heart, complicating recovery and treatment.
- Surgical Risks: The surgery to repair the diaphragm is delicate and can lead to complications such as infections, bleeding, or damage to surrounding organs.
- Gastrointestinal and Nutritional Issues: The displacement of abdominal organs can affect gastrointestinal function, leading to feeding difficulties, reflux, and growth concerns.
Long-term Outlook and Potential Developmental Concerns
While many children who undergo treatment for CDH can lead healthy lives, the condition can have lasting effects that extend into childhood and beyond. The long-term outlook for children with CDH depends on the severity of the hernia, the presence of other birth defects, and how well their lungs have developed. Potential long-term and developmental concerns include:
- Chronic Lung Disease: Children who have had CDH may experience ongoing respiratory issues, such as chronic lung disease, which can affect their physical activity levels and quality of life.
- Neurodevelopmental Delays: There is an increased risk of neurodevelopmental delays in children with CDH, possibly due to the initial lack of oxygen or complications from treatment. These can include challenges with learning, motor skills, and speech.
- Hearing Impairment: Some children treated for CDH may experience hearing loss, necessitating regular hearing evaluations as they grow.
- Growth and Nutritional Challenges: Ongoing gastrointestinal issues can lead to difficulties in gaining weight and growth, requiring careful monitoring and management.
The journey for infants with Congenital Diaphragmatic Hernia is fraught with challenges, from immediate post-birth complications to long-term developmental concerns. However, with advancements in medical treatment and a multidisciplinary approach to care, the prospects for these children continue to improve. Early intervention, regular follow-up, and supportive care are crucial to address the multifaceted needs of children with CDH, helping them to achieve their full potential.
Advancements in Congenital Diaphragmatic Hernia Treatment
Advancements in the treatment of Congenital Diaphragmatic Hernia (CDH) have marked a significant turning point in how this condition is managed, offering new hope and improved outcomes for affected infants. Recent research findings and the advent of emerging treatments have played a pivotal role in these advancements.
Recent Research Findings and Emerging Treatments
The landscape of CDH treatment has been significantly reshaped by recent research, which has introduced innovative approaches and technologies. These advancements include the development of new surgical techniques, the application of regenerative medicine to repair the diaphragm, and the use of advanced ventilator strategies to improve respiratory outcomes for newborns. Furthermore, the exploration of prenatal therapies aimed at stimulating lung growth and development has opened up new avenues for early intervention. These emerging treatments are not only focused on repairing the hernia but also on addressing the pulmonary hypoplasia and pulmonary hypertension that often accompany CDH, thereby improving the overall survival and quality of life for these patients.
The Role of Fetal Surgery and Outcomes
Fetal surgery for CDH represents one of the most remarkable advancements in the field. This approach involves repairing the diaphragmatic hernia before birth, offering the potential to improve lung development and reduce the severity of respiratory distress after delivery. Studies have shown that fetal surgery can lead to better outcomes in selected cases, particularly for fetuses with a severe prognosis based on prenatal imaging and diagnostic criteria. However, fetal surgery is complex and carries risks for both the mother and the fetus, necessitating careful consideration and selection of candidates based on rigorous criteria.
The outcomes of fetal surgery for CDH have been encouraging, with improved survival rates and reduced need for postnatal interventions in some studies. Nonetheless, long-term follow-up is essential to assess the impact on respiratory function, neurodevelopment, and overall quality of life. The ongoing research and clinical trials continue to refine the criteria for fetal surgery, improve surgical techniques, and better understand the long-term outcomes of this innovative treatment approach.
However, the advancements in CDH treatment, particularly through recent research findings and the pioneering role of fetal surgery, have significantly improved the outlook for affected infants. These developments underscore the importance of ongoing research, multidisciplinary care, and personalized treatment strategies to optimize outcomes for patients with CDH.
Preparing for Your Child’s Care
Preparing for your child’s care when dealing with Congenital Diaphragmatic Hernia (CDH) requires thoughtful planning and support. Here’s how to ensure you’re well-prepared:
Choosing the Right Healthcare Team and Facility
Selecting an experienced healthcare team and facility that specialize in treating CDH is crucial. Look for hospitals with a high volume of CDH cases and specialized neonatal intensive care units (NICUs). These facilities often have the most experienced teams and the latest treatment options available. Don’t hesitate to ask about the healthcare professionals’ experience with CDH and the outcomes of their treatments.
What to Expect Before, During, and After Treatment
- Before Treatment: Expect several consultations with your healthcare team to understand the diagnosis, treatment options, and outcomes. This may include detailed ultrasounds, MRI scans, and discussions about the timing and type of surgery your child may need.
- During Treatment: If surgery is needed, it usually occurs after your baby is stabilized post-birth. Your medical team will keep you informed about the procedure and how your child is doing.
- After Treatment: Post-surgery, your child will likely need to stay in the NICU for monitoring and care. The length of this stay can vary depending on the severity of the CDH and the surgery’s success. Follow-up appointments will be crucial for monitoring your child’s development and health.
Support Resources for Families Affected by CDH
Navigating CDH can be challenging, but you’re not alone. Many hospitals offer support groups for families dealing with CDH. These can provide emotional support and practical advice from families who have been through similar experiences. Additionally, online communities and non-profit organizations dedicated to CDH can offer resources, education, and connections to further support. Engaging with these communities can provide a valuable network of support and information.
Remember, the journey with CDH is unique for every child and family. Being well-informed and supported by a strong healthcare team and community can make a significant difference in managing your child’s condition effectively.
FAQ Section: Understanding Congenital Diaphragmatic Hernia (CDH)
What is Congenital Diaphragmatic Hernia (CDH)?
Congenital Diaphragmatic Hernia (CDH) is a birth defect characterized by an abnormal development of the diaphragm, the muscle that separates the chest from the abdomen. This condition allows abdominal organs to move into the chest cavity, affecting lung development and function.
How is CDH diagnosed?
CDH is often diagnosed before birth through prenatal ultrasound, which can show the herniation of abdominal organs into the chest cavity. After birth, diagnosis may be confirmed through imaging tests such as X-rays, MRI, or CT scans to visualize the position of organs and the diaphragm.
What are the treatment options for CDH?
Treatment for CDH typically involves surgical repair of the hernia, which may be performed after the baby is stabilized. The timing of the surgery can vary based on the baby’s health and the severity of the condition. In some cases, advanced therapies like ECMO (Extracorporeal Membrane Oxygenation) may be used to support the baby before and after surgery.
Can CDH be detected during pregnancy?
Yes, CDH can often be detected during pregnancy with a prenatal ultrasound. This allows for early planning and intervention, including the consideration of delivering at a hospital with a neonatal intensive care unit (NICU) and specialists experienced in treating CDH.
What is the prognosis for babies with CDH?
The prognosis for babies with CDH can vary widely depending on several factors, including the size of the hernia, whether other anomalies are present, and the baby’s overall health at birth. Advances in medical and surgical care have significantly improved outcomes, with many children leading healthy lives.
Are there long-term effects of CDH?
Some children born with CDH may experience long-term effects, such as respiratory problems, gastrointestinal issues, or developmental delays. Follow-up care with a multidisciplinary team is essential to address any ongoing or emerging health concerns.
Can CDH be prevented?
Currently, there is no known way to prevent CDH. Research is ongoing to understand the causes of CDH, which may lead to preventive strategies in the future. However, obtaining appropriate prenatal care can help in early detection and planning for treatment.
Conclusion:
In wrapping up our discussion on Congenital Diaphragmatic Hernia (CDH), it’s crucial to underline the significance of early diagnosis and the implementation of effective treatment strategies. CDH, a condition present from birth that affects the diaphragm’s development, can lead to significant respiratory distress and other complications in newborns. Early detection through prenatal screenings and advances in medical imaging can pave the way for timely interventions, significantly improving the survival rates and quality of life for affected infants.
Effective treatment for CDH often involves surgical repair of the hernia, coupled with supportive care to manage respiratory and nutritional needs. The advancements in neonatal care and surgical techniques have dramatically enhanced outcomes, emphasizing the importance of specialized care for these vulnerable patients.
Moreover, ongoing research into the causes, treatment options, and long-term outcomes of CDH is indispensable. Support for clinical trials and studies can contribute to a deeper understanding of the condition, leading to innovative treatment approaches and improved patient care protocols. The commitment of healthcare professionals, researchers, and support groups to advancing our knowledge and treatment of CDH is crucial for continuing to improve the lives of those affected.
We encourage patients, families, and the medical community to advocate for and support ongoing research in CDH. Together, through education, research, and compassionate care, we can make a significant difference in the lives of those touched by congenital diaphragmatic hernia.